
Over the last three decades I’ve had the pleasure of working with those in the adult social care sector at all levels. I learnt that compassion, resilience and a sense of humour are qualities that all those I met had in common. They are required to be trustworthy, reliable, open-minded and flexible, often in challenging circumstances, and they don’t always receive the recognition they deserve.
If you ask anyone who works in Adult Social Care “is your sector better or worse than it was 10 years ago?” they will almost definitely say “worse”. Their reasons being funding cuts, increase in demand and workforce shortages. But is there optimism about the future?
Over the past decade the adult social care sector has undergone significant changes, shaped by evolving demographics, policy shifts, technological advancements, and social changes. Some of these changes have brought challenges to the sector and others have brought opportunities. Well, let’s look at what has happened in the last decade and what the landscape might look like in the future.
Challenges
Demographic Changes
It’s not news that there is an ageing population in the UK. In 2024, there were approximately 22 million people aged over 50 in England, accounting for two in five of the total population. This number is rapidly increasing, with projections indicating a 19.3% rise between 2024 and 20441. By 2036 the over 85 age group is expected to reach 3.5%, (2.6 million), of the total UK population2 and the number of people requiring long-term care is projected to rise significantly.

As people live longer, the risk of developing age-related conditions like dementia increases. Around 1 million people in the UK are living with dementia and this number is projected to rise to 1.4 million by 20402. The increase is partly down to improved diagnosis, but also other conditions such as heart disease and stroke have declined, meaning more people are getting to an older age when they are more likely to develop dementia.
Other complex needs are increasing, such as diabetes and mobility issues requiring more integrated and person-centred care. In 2010, approximately 2.9 million people in the UK were diagnosed with diabetes. This increased to 4.4 million by 2022/23 with an additional 1.2 million people potentially living with undiagnosed type 2 diabetes, bringing the total to around 5.6 million4. Projections suggest that diabetes prevalence in the UK could reach 5.3 million by 20255.

Among working-age adults with disabilities, approximately 41% reported mobility impairments in 2022/23. This number increases to approximately 45% for those over the State Pension age and for those aged 85 and over the number increases to 67%6.
All of the above factors place a greater and greater demand on adult social care services.
Policy and Funding
Since the early 2010s, local authority funding for adult social care has faced significant cuts as a result of austerity policies. Between 2010 and 2020, spending on social care fell by 12% in real terms despite increasing demand.
Numerous proposals for reforming adult social care funding were debated in the last decade, but not implemented, however the following have been:
- Social Care Levy
In 2022, the government introduced a National Insurance increase, dubbed the “Health and Social Care Levy,” intended to address some of the funding challenges. However, debates continue about its adequacy. - Integrated Care Systems (ICS)
The NHS and social care sectors moved toward closer integration through the introduction of ICS in 2022. The aim to streamline health and social care services at the local level. While it’s still relatively early to definitively say whether ICSs have fully achieved their goal of streamlining health and social care services at the local level, there are indications of some progress but there are challenges, including adequate funding, as well as benefits. So really, it’s watch this space. - Preference for Ageing in Place
Prior to the late 20th century ‘Ageing in Place’ has been discussed, but it has gained momentum over the last decade, with a shift away from residential care. It has resulted in greater investment in domiciliary (home-based) care services. However, there are professionals in the sector that feel that ‘Ageing in Place’ has not been sufficiently examined to consider the connection between Ageing in Place and the changing experience of ‘home’ over time8. - Support for Carers
Unpaid carers in the UK provide an estimated £132 billion worth of care annually. Policies have sought to provide more recognition and support, such as the Carers’ Allowance and initiatives for respite care, although critics argue that funding and support remain inadequate. - Carers UK Advocacy
Organisations like Carers UK have successfully lobbied for increased acknowledgment of carers’ rights, including improved workplace flexibility.
The sector has always been a political football and the lack of clarity on long-term funding mechanisms has left the sector in a precarious position.
Access to Care
Over the last decade we have seen that access to social care varies significantly across the UK, due to the wealthier local authorities being able to provide more services, while poorer one’s face constraints.
The means-tested system, which came into effect in 1948 and has had many changes since, has left some individuals unable to afford care, while others are forced to sell assets, including homes, to pay for services. For information on changes to the means-tested system go to The House of Commons Library.

Staffing
The adult social care workforce in the UK has faced severe shortages, made worse by Brexit and reducing the number of European Union care workers, as well as the Covid pandemic. By 2023, the sector reported over 160,000 vacancies, but with care workers wages being at or near the minimum wage and media reported low morale, recruitment has been extremely challenging.
In light of the staffing challenges there have been steps to professionalise the adult social care sector over the last decade. Training has been one such step, with the introduction of the Care Certificate in 2015, requiring new care workers to gain a basic knowledge and skills. Further mandatory training is required by those who work in the sector, the Skills for Care Mandatory Training Guide, sets out the requirements, e.g topic and frequency of re-training.

NVQs and apprenticeships have also been promoted in an attempt to get more qualified individuals into the sector. However, apprenticeships, an area I worked for many years, those starting an adult social care apprenticeship in 2022/23 decreased by 14% on the previous year. At the peak in 2016/17 there were around 99,200 starters. For more information on apprenticeship data go to Skills for Care.
To attempt to improve standards, the Care Quality Commission, which inspects and rates social care providers, underwent significant changes with the aim of improving its services. In 2023 the Single Assessment Framework, SAF, was introduced which aimed to simplify the assessment process and make it more focused on key areas of quality. However, despite this, a 2024 review to find out the operational effectiveness of the CQC9 found:
“Significant failings in the internal workings of CQC, which have led to a substantial loss of credibility within the health and social care sectors, a deterioration in the ability of CQC to identify poor performance and support a drive to improve quality – and a direct impact on the capacity and capability of both the social care and the healthcare sectors to deliver much-needed improvements in care”.
Benefits, but with Challenges
Technological Advancements
Over the past decade, technological advancements have significantly transformed adult social care. However, these advancements have been met with mixed reactions with those who work in the sector. Some have welcomed the potential benefits of technology, such as improved efficiency and communication, but others have been less positive.
There have been concerns about data privacy, the cost of implementation, and the lack of adequate training and support. There have been concerns about data privacy, the cost of implementation, and the lack of adequate training and support.

Some of the technological advancements have without doubt brought improved accessibility to care and the ability to live more independently. Technology such as:
- smart home systems
- voice activated assistants
- wearable technology, which can detect falls
- remote monitoring devices, which can detect motion
- virtual consultations, which allow individuals to receive care from their homes, reducing hospital visits
- emergency alarms which provide immediate assistance to those with mobility issues or chronic conditions
- Telehealth platforms, which enable regular check-ins with healthcare professionals without the need for physical travel.
All these technological advancements are improving independent living, and outcomes and satisfaction for individuals
The increased use of data-driven care management platforms provide data and analytics enabling care providers to offer proactive care and tailored support for individual needs. Digital care plans can be personalised and offer seamless communication among care providers, improving continuity and co-ordination of care. The care management software also reduces administrative burdens, assisting with scheduling and documentation, and improves management reporting to aid with compliance.
Despite there still being some resistance to the use of technology in adult social care there have been some very successful programmes to teach those who work in the sector how to use technology. But, this challenge remains and as technology continues to increase in use more training will be required. There are also concerns around privacy and security, in particular cyber threats, and ethical considerations especially as the use of artificial intelligence, AI, increases.
Cutting-edge technologies are not inexpensive and not all care providers or individuals can afford the cost, creating disparities in care delivery and access.
The Future
Certainly, the UK government’s ongoing debates around funding and reforms are likely to shape the future of adult social care. The continued integration of health and social care services under ICS and advancements in technology offer opportunities to improve care delivery, though challenges such as funding and workforce sustainability remain. So the sector is likely to have a growing focus in the coming years on environmental sustainability within care homes, the introduction of new technologies and staff training.
But what about funding? Well, projections indicate substantial financial pressures in the coming years; no change there then, I hear you say! To meet demand, funding in England would need to increase by 3.4% per year in real terms up to 2032/33, according to the Institute for Fiscal Studies11. This is significantly higher than the average real growth of 0.7% per year we’ve seen over the last decade. Going forwards, the UK government has said it will commit to investment and reforms of the sector and support for the workforce. They have announced up to £3.7 billion of additional funding for social care authorities in 2025 to 202612. However, experts like the Health Foundation predict a much larger funding need in the coming decade to adequately meet growing demand, potentially reaching £18 billion by 2032/3313.
Some sources suggest that technology has the potential to significantly impact adult social care in the next decade. This is likely to include further advancements in remote monitoring, the increased use of AI-powered tools to assist with everyday tasks like care planning and risk assessment.
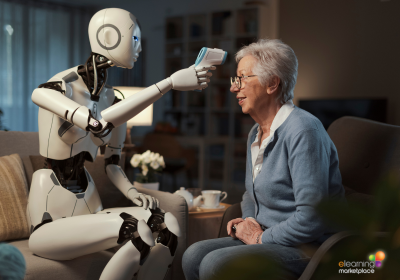
Robotics, which are already in use, are set to become more common place, helping with physical tasks like lifting and mobility, social interaction and emotional support and reducing loneliness. Virtual reality (VR) and augmented reality (AR) could be used for training, rehabilitation, and providing social interaction and engagement. Continued development of assistive technologies are likely to help individuals with disabilities maintain independence and live more fulfilling lives.
We will see data analytics and predictive modelling help to identify patterns and predict future needs, including workforce planning, resource allocation, service demand and demographic insights allowing for more proactive and personalised care. Digital platforms are likely to be used more for mental health support providing resources, mindfulness tools and virtual therapy sessions.
The UK Government has said that in 2028 they will make long-term recommendations for the transformation of adult social care. So, the next decade looks like another one of changes and challenges, and one that we’ll almost certainly see innovation at its heart. Technology has the potential to transform adult social care in the next decade, but it’s important to approach these advancements thoughtfully and responsibly to ensure that they benefit both individuals receiving care and those who provide it. With the general sentiment being one of concern and apprehension among those working in adult social care, the next decade still has a lot of work to do to turn that concern into optimism.
Author: Carolyn Lewis
Sources:
- https://www.ageuk.org.uk/discover/2024/september/state-of-health-and-care-of-older-people-in-england-2024
- https://www.beta.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2021basedinterim
- https://www.alzheimers.org.uk/about-us/policy-and-influencing/local-dementia-statistics
- https://www.diabetes.org.uk/resources-s3/2017-11/diabetes_in_the_uk_2010.pdf
- https://www.diabetes.co.uk/diabetes-prevalence.html
- https://commonslibrary.parliament.uk/research-briefings/cbp-9602
- https://www.statista.com/statistics/860984/disability-prevalence-impairment-united-kingdom-uk-by-age-group/
- https://journals.sagepub.com/doi/10.1177/13607804221089351?icid=int.sj-abstract.citing-articles.11
- https://www.gov.uk/government/publications/review-into-the-operational-effectiveness-of-the-care-quality-commission-full-report/review-into-the-operational-effectiveness-of-the-care-quality-commission-full-report
- https://commonslibrary.parliament.uk/research-briefings/cbp-8005/
- https://ifs.org.uk/publications/adult-social-care-england-what-next
- https://www.gov.uk/government/news/new-reforms-and-independent-commission-to-transform-social-care
- https://www.health.org.uk/reports-and-analysis/analysis/social-care-funding







 UK: 0844 854 9218 | International: +44 (0)1488 580017
UK: 0844 854 9218 | International: +44 (0)1488 580017








